
Talking to those close to you about your wishes, values, and beliefs is a crucial part of planning for your future health care and personal care.
Your body is your business. It’s important that you’re able to control what happens to it — now and into the future. One day you might be unable to make decisions for yourself. Learn what you can do to ensure your wishes around health care and personal care are always respected.
What you should know
Putting a plan in place now gives you a say in your future health care and personal care decisions. This is called advance care planning. It’s a process where you think about and share your values, beliefs and wishes, to support informed health care and personal care decision-making. This gives you the best chance of getting care that’s right for you.

The process of planning can help you to:
understand your medical options
explore your values and preferences
help those close to you understand what you want
prepare you, or those close to you, to make difficult decisions in a health crisis
While you can still make your own decisions
As long as you can still make your own decisions, your advance care plan won't be used. It only comes into play when you can no longer say, with full understanding, “yes” or “no” to receiving health care or personal care.
The options we describe below are ways in which you can have a say in your future health care and personal care.
What will I wear today?
Who will I spend time with?
Where will I live?
We all make personal care decisions every day. In addition to choices about clothing, connections, and living arrangements, personal care also includes diet, social activities, exercise, where you work, and spiritual matters.
Should I have this surgery?
Is this medical treatment worth the risk?
Do I want to be kept alive at all costs, or allowed to die naturally?
Health care decisions also have a huge impact on our quality of life. The answers can have huge consequences. Big and small health care decisions are covered. Minor health care includes routine tests, dental and eye work, and medication. Major health care includes major surgery, chemotherapy, dialysis, complex diagnostic tests, and risky treatments.
“I thought my sister Jayne knew me pretty well — we’ve always been close. But our conversation about our values and preferences for health care treatments was eye-opening. I’m glad Jayne now knows what’s important to me at end-of-life. She can make decisions for me according to my values and not her own!”
– Lily, Vancouver, BC

You may believe those close to you know what matters to you most — but they may not. When someone makes a decision for care on your behalf, it’s important that they know your wishes, beliefs, and preferences for care. This will help them to make care decisions that align with your wishes and values.
Health care decisions
In BC, there are various laws that require different kinds of decision-makers to specifically consider your instructions, wishes, values, beliefs, and preferences for care when making a health care decision for you.
Personal care decisions
Your values, beliefs, and preferences will also influence what personal care you’d want to receive in the future.
For example, imagine someone who’s been given an initial diagnosis of Alzheimer’s. They know that some day, inevitably, their disease will progress. It will probably get so bad that at some point, they won’t even recognize their family. With all this in mind, they might have a strong preference that they’d never want to be spoon fed for an extended period of time, once they’re in the advanced stages of the disease. This may be due to cultural, spiritual, or religious values, or simply a personal belief about what “quality of life” means to them. This kind of care (that is, assisted feeding to provide nutrition or hydration) falls under personal care.
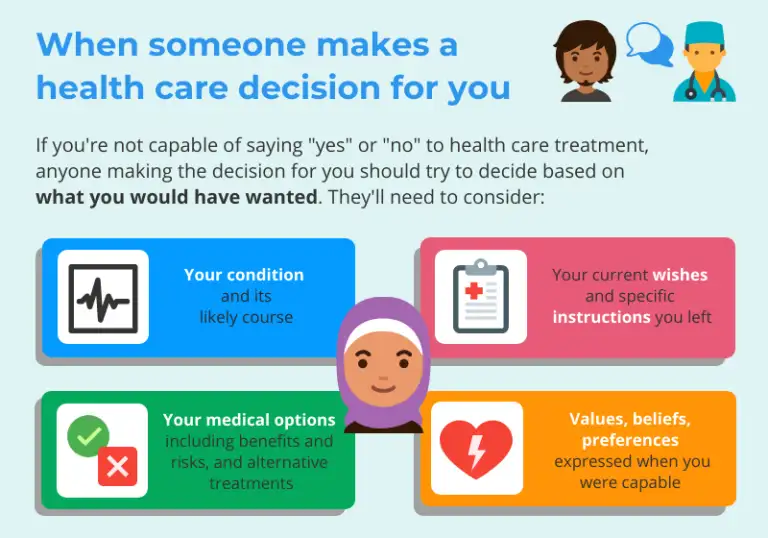
If you’re incapable of consenting to medical treatment, someone else needs to make the decision about whether to give or refuse consent. There’s a hierarchy of authority that a health care provider must follow if a health care decision needs to be made and you’re not able to make it. The visual below steps through this decision-making hierarchy.
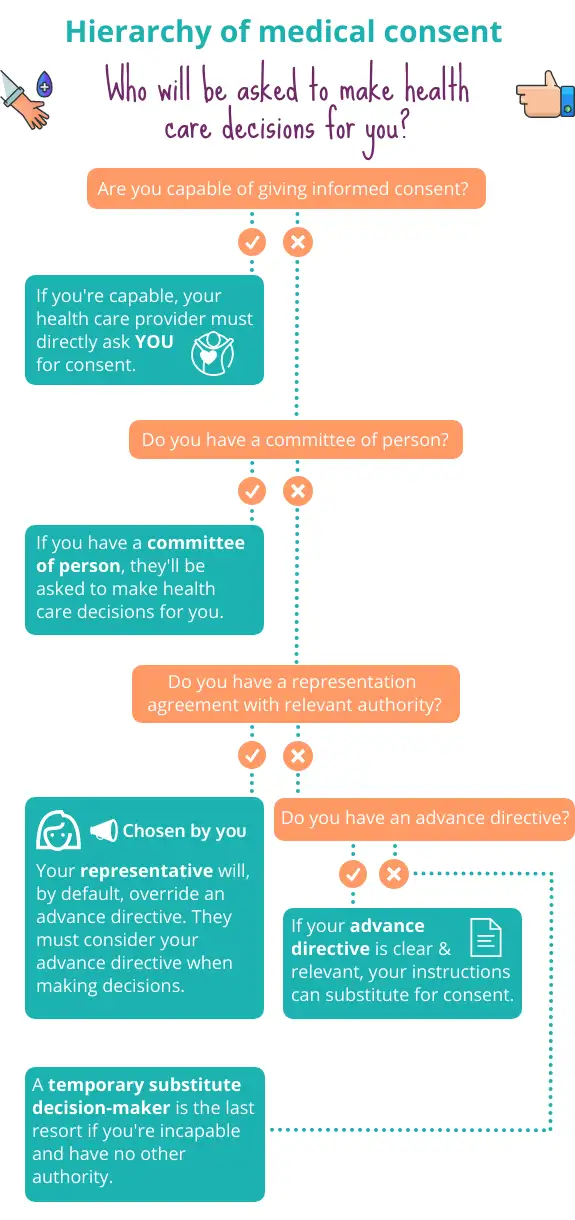
Each type of authority is explained in more detail below.
Who can make decisions for your health care
At the bottom of the hierarchy is a temporary substitute decision-maker.
This person will be temporarily appointed to make a specific health care decision for you. They’ll only be called on if you don’t have another authority in place that addresses the specific health care need. Unlike other authorities which you can choose in advance, a temporary substitute decision-maker is not someone chosen by you — it may be someone you never would have wanted to make a decision about your health for you.
To choose a temporary substitute decision-maker, your health care provider must choose someone from a ranked list, as set out under the law. Learn who might be chosen and what they’ll be asked to do.
“My grandpa is 94 and has severe dementia. He needs help with everything: walking, eating, bathing, dressing. Before he got sick, he told me ‘Don’t let them tube feed me for any prolonged period of time. That’s no way to live!’ As his chosen representative, I can talk with his care home about the kind of personal care he would have wanted. I can also make health care decisions, as they arise.”
– Ali, West Vancouver, BC

An enhanced representation agreement (often called a section 9 representation agreement) lets you choose someone to make legally binding health care and personal care decisions for you. The person you choose is called your representative. They can help you to make health care and personal care decisions, or make decisions for you, if you ever become incapable of making these kinds of decisions for yourself.
There are many advantages to choosing a representative over falling back on a temporary substitute decision-maker.

Even if you have a representation agreement in place, a doctor or other health care provider must always check with you before taking any action. If you’re capable of making the decision yourself, they must obtain informed consent from you. Your representative can’t override your decisions as long as you’re still capable.
There are two types of representation agreements
An enhanced representation agreement is usually appropriate for most capable adults. A standard representation agreement is often used as a last resort when someone already has a diminished capacity to understand. We can help you figure out which type of agreement is the right fit for you.
“I was born with a gene that gives me a coin-flip’s chance of getting Huntington’s Disease. It’s a horrible, incurable affliction, and if I get it I frankly don’t want to suffer like my mom did. After consulting with both my family doctor and a lawyer, I’ve signed an advance directive saying: if I test positive for Huntington’s, I want certain things to happen — and not happen — in my end-of-life care.
– Rory, Phillips Arm, BC

An advance directive is a legal document where you record your wishes around accepting or refusing specific health care treatments.
If you’re incapable of giving or refusing consent to health care, your health care provider may seek consent to treatment from your advance directive. They must honour the advance directive where it refuses consent.
There are some exceptions. For example, your health care provider can not follow your advance directive if your instructions:
are so unclear they can’t be understood or applied, or
are irrelevant to the medical situation at hand.
Is this the right fit for me?
If an advance directive isn’t clear, specific, and relevant to the medical situation at hand, it may be ineffective when needed most. For this reason, advance directives are best used when someone:
has a specific diagnosis,
is at end-of-life, or
is trying to get ahead of a condition they are genetically predisposed to and have seen others close to them go through.
In all of the above cases, a doctor would be able to explain the specific medical treatments or interventions likely to be offered to the patient. In this way, a patient can make truly informed decisions.
Prepare an advance directive
We walk you through preparing an advance directive, and explain when an advance directive can’t be used.
If you were to become incapable and you’d neglected to put an authority in place, someone may need to apply to the court to make decisions for you. They are asking the court to appoint them to be your committee of person. A committee of person has broad powers to make health care and personal care decisions for you.
This may be necessary when:
a major health care decision or action needs to be made on your behalf,
there’s no representation agreement or advance directive in place, and
a temporary substitute decision-maker can’t be located or there’s a family disagreement.
The person who applied will be appointed as your commitee, if the court approves their application.
Make your advance care plan
Planning isn’t just about signing legal documents. Any tool you choose to use will be most effective if those close to you and health care providers know what you want.
These resources can help you think about your values and start conversations about them. The process of writing down your values and wishes can clarify, in your own mind, what’s important to you.

Advance Care Planning Canada
Provides an online workbook to help you make your advance care plan.
My Voice: Expressing My Wishes for Future Health Care Treatment
A guide to making your advance care plan, including a workbook and legal forms.
Talk to your health care provider
Your planning will be most useful if you have an understanding of your condition, how it might progress and what your health care needs might be as it does. Talk to your care providers to learn about any conditions you have and the specific treatments that might be offered to you.
Specific questions you should ask your health care providers are:
How might my illness progress?
What are the possible complications I might experience?
What treatment decisions might I have to make in the future?
What are the risks and benefits of certain medical interventions I might receive? For example: What does CPR entail? What are the risks? How might it impact quality of life?
Learn about your legal options
You’re learning about your legal options by reading this page! These options, such as preparing a representation agreement or advance directive, don’t exist in a vacuum. Whatever combination of options you choose, you should think about each option in the context of your own values, wishes and beliefs.
An enhanced representation agreement is typically appropriate for most capable adults. Choosing your representative is an important decision and it's not always easy. Most people ask a family member or close friend. Think about what you’re asking of your representative and who might be up for the job. This should be someone you trust with your life — literally! And it should be someone who you know will ensure that your needs and wishes — not theirs — come first.
If you’re ready to start planning, our coverage of preparing an enhanced representation agreement explains the factors to consider when choosing a representative, and takes you step-by-step through preparing the document. It also explains how this kind of agreement works, and your legal rights.
You can choose more than one representative
For example, you can choose two or more people (such as a group of family members) to make decisions for you, or to help you make decisions.
None of us can know precisely what health challenges we’ll face down the road. This is especially true for healthy adults with no red flags in their family history. This makes conversations about general values (“I’m most concerned about losing quality of life”) and preferences (“I do not want to be hooked up to machines”) useful for healthy adults.
The best place to begin having these conversations is before a health crisis hits — around the dinner table, rather than at the intensive care unit!
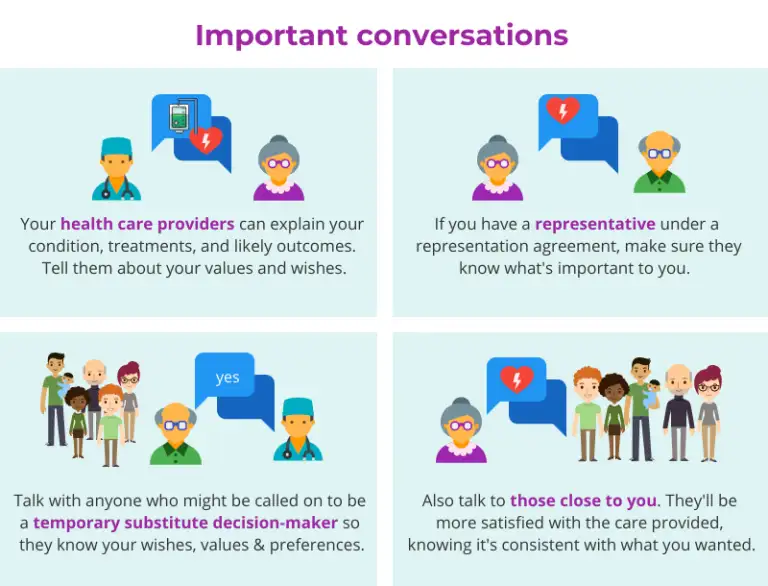
Have these conversations with:
your family and those who are close to you,
anyone who might be asked to make a decision for you, and
your health care providers.
Be clear about what these kinds of statements really mean to you. To do this, learn as much as you can about the possible health care treatments that might be offered to you at end-of-life from your health care provider.
These conversations will give you the opportunity to make sure that your wishes are expressed and respected. They’ll help to ensure there’s a shared understanding of what matters most to you when it comes to personal care and health care, including end-of-life care. The information will be helpful to someone who has to unexpectedly make a decision for you because of a sudden accident or illness.
It’s not always easy to talk about these kinds of things. Here are some ideas of what you could say to break the ice:
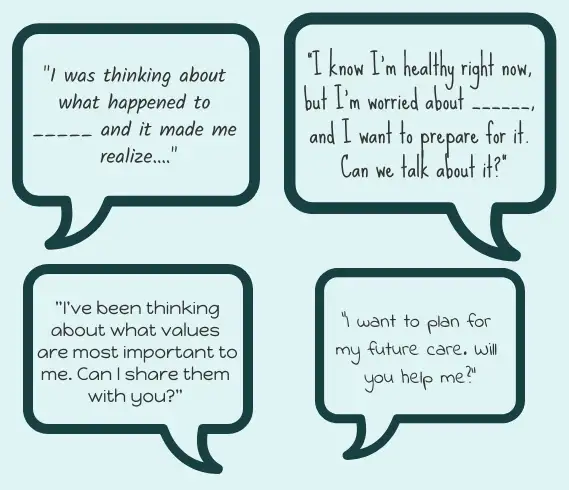
The visual below depicts some of the important conversations you should have as part of the planning process.
You have a number of options. Any combination of these options may be the right fit for you, depending on your circumstances and preferences.
Fill out an advance care plan or values guide. It’s a good idea to write down your wishes, or make a recording. Thinking about your values and wishes is a crucial part of planning. The information will help guide anyone who has to make a decision for you. Be aware, though, that a completed values guide cannot substitute for your consent if you’re incapable. On the other hand, if you prepare legal documents, your health care provider can legally get consent from your advance directive or representative.
List any potential temporary substitute decision-makers. It’s a good idea to write down the details of everyone who might potentially fall into this role. Give these details to your health care provider. The list should include each person’s name, their relationship to you, and how to best contact them. Everyone should do this. We have detailed guidance to help you. Doing this will save your health care provider valuable minutes, maybe even hours, when a medical decision needs to be made on your behalf. Even if you have a representation agreement, writing these details down acts as a back-up plan. For example, your representative might not be available.
Choose someone to speak for you with an enhanced representation agreement. We provide step-by-step instructions on how to prepare one.
A thought experiment
Think about every person in your life who could potentially be contacted to be a temporary substitute decision-maker (including siblings, parents, and any other relative). Would you ever want them to make a critical health care decision for you? If the answer is “no,” you should think about preparing a representation agreement.
If you have a specific diagnosis, record your instructions for care with an advance directive. Learn what's involved in preparing an advance directive.
Keep in mind it's only a piece of paper
If you prepare an advance directive, it’s a good idea to have a representation agreement too. An advance directive is a piece of paper. It can’t advocate for you, give context to health care providers, or be responsive to changing situations. These are things that a well-informed representative who knows your medical history as well as your values and wishes can do.
You can choose to nominate a committee of person. While you’re still legally capable, you can nominate a particular person to be your committee. You can’t actually appoint someone yourself — a nomination is simply a way of communicating your preference to the court. Be aware that obtaining committeeship is the most intrusive planning option. Legally, you lose your decision-making rights. A committee of person may work for you if you have someone you trust who you believe could represent your interests well, and you prefer that your decision-maker is appointed by the court, or you think there could be family conflict if a committee ever needed to be appointed.
As things change
If your circumstances or condition changes, you should revisit any documents you’ve prepared. Your conversations can now focus on what you want in the context of your condition.
Common questions
A MOST form — which stands for medical orders for scope of treatment — is a document used in hospitals, residential care, and community care settings. It should be used to facilitate a conversation with your doctor about your values and wishes for care. You may encounter a MOST when you’re chronically ill or near end-of-life, and major health care decisions are looming.
Legally, MOST forms do not substitute for consent. Even if you have a MOST, they must ask you directly for your consent to medical treatment (there are some exceptions in emergency situations). If you’re incapable of giving consent, they need to get consent from your substitute decision-maker. Otherwise, they cannot treat you. What’s written in a MOST form should never override this consent process.
If your heart or lungs suddenly stop working, cardiopulmonary resuscitation (CPR) or other emergency medical procedures are usually performed straight away. A no CPR form can be used to tell first responders you don’t want so-called heroic measures undertaken.
The form was created by the BC Ministry of Health. Instructions for how to create a no CPR form can be found on HealthLinkBC. There’s no law in BC that governs the creation and use of no CPR forms. The reality is these forms are used in the BC health care system and honoured by health care providers.
Signing a no CPR form isn’t a decision to be made lightly. Talk to close family and friends and your doctor to see if it’s a good option for you. This will depend on your unique circumstances.
A MOST form and a no CPR form will be honoured by BC Emergency Health Services in an emergency situation. If you have either form, you should post a copy on your fridge. If you have decided on no CPR, you should wear a MedicAlert® or CPR bracelet or necklet to enable quick verification that you have a no CPR form. To obtain a free no CPR bracelet or necklet, call 1-800-668-1507 or visit the Medic Alert website.
The way decisions are made within families varies from culture to culture. Some of the suggestions above may be new to you.
The laws in British Columbia emphasize an individual's right to make their own decisions about their own care. This may not be the way things are typically done in your family. But the laws apply to you, so learning about them can benefit you and your family.
If you become incapable, your health care decisions will need to be made by someone else, on your behalf. Say you have no plans in place. By default, your health care provider will need to contact a temporary substitute decision-maker, to make the decision for you. This person will be chosen from a ranked list. Your health care provider only needs to get consent from one person on the list.
Representation agreements are flexible. You can choose one or more people to make decisions for you, or to help you make decisions. If you choose a representative(s) in advance, you can tell them how you’d like decisions to be made. For example, you can tell your representative that they must consult with other family members about major medical decisions.
As long as you're capable of making a health care or personal care decision when it arises, your advance care plan won't be used. It’ll be up to you to accept or refuse treatment or care. It’s a good idea to review your plan at least once a year and whenever your circumstances change. Make sure your representative is still up to the task. Update your documents and give out new copies if your plans change.
A representative under a representation agreement can speak for you, or help you speak up for yourself, on personal care matters. Personal care under a representation agreement can include:
what you eat
where you live
social activities and contact with others
exercise
arranging support services
personal safety
Personal care becomes especially important if you develop a chronic illness or a condition like dementia, or you’re moving into a care facility.
Advance directives and temporary substitute decision-makers only cover health care matters.
Who can help

BC Centre for Palliative Care
Provides resources for individuals and families to understand palliative care and advance care planning.

Nidus Personal Planning Resource Centre & Registry
Detailed information on personal planning, including template forms.

Advance Care Planning Canada
Provides an online workbook to help you make your advance care plan.


